My Cognitive Dissonance with PRI
Last month I took my first Postural Restoration Institute course entitled Myokinematic Restoration. For those who are unfamiliar with Postural Restoration Institute (PRI), the best way I can describe it is that it is an approach that focuses on correcting natural physical imbalances of the body that lead to asymmetrical patterns of movement dysfunction. First developed by physical therapist Ron Hruska in 2000, I had been hearing more and more about PRI in recent years and noted that many rehabilitation professionals whom I respect and whose written content I follow employed its usage. I felt like it was gaining more and more popularity in both the rehabilitation and personal training worlds, and also that there seemed to be some anecdotal controversy regarding its foundations and principles. Up until now I had only read reviews of various PRI courses and believed I needed to take a course firsthand to draw my own conclusions regarding their methods. Like most continuing education courses these days, the subject material and basic PRI philosophy was also not covered in my physical therapy school. After the course ended, I don't think I've ever experienced such cognitive dissonance over a rehabilitation approach before--I wanted to accept PRI wholeheartedly but it was hard for me to do so at the end of the weekend. This following post will be my personal review of the course and I'll flesh out my thoughts regarding stuff I liked, stuff I didn't like so much and some stuff in between.
What is Myokinematic Restoration, Anyway?
Myokinematic Restoration is one of the three "primary courses" offered by PRI which serve as introductions to their philosophy and must be taken before delving into their more advanced coursework. The following course description is from the PRI website:
“This advanced lecture and lab course explores the biomechanics of contralateral and ipsilateral myokinematic lumbo-pelvic-femoral dysfunction. Treatment emphasizes the restoration of pelvic-femoral alignment and recruitment of specific rotational muscles to reduce synergistic predictable patterns of pathomechanic asymmetry. Emphasis will be placed on restoration, recruitment, and retraining activities using internal and external rotators of the femur, pelvis, and lower trunk”
I probably read this a dozen times when I was considering signing up for this course before feeling like I understood it! In a nutshell, the Myokinematic Restoration course is based on several physiological facts or assumptions (not an exhaustive list):
- In general, most people have a dominant postural presentation called the Left Anterior Interior Chain (LAIC) pattern: The left pelvis is anteriorly tipped and forwardly rotated (in the transverse plane).
- Other common presentations as a result of the LAIC include elevated anterior ribs on the left, depressed shoulder/chest on the right, posterior rib hump on the right and overdeveloped lower right back muscle.
- Muscular fibers of the diaphragm extend more inferiorly upon the right side of the anterior lumbar spine and predispose us posturally to rotate to the right.
- Our livers are positioned on the right side of our body which also contributes to this directional rotational pull to the right side.
- The left side of the diaphragm which is much smaller than the right cause the abdominal muscles on the left side to become weak.
I was aware of some of these anatomical observations from my cadaver dissection labs in grad school, but never have I encountered a school of thought in which predisposed movement asymmetries based on these were so discretely defined. These observations were established early in the course and served as foundations for more advanced concepts and treatment rationales.
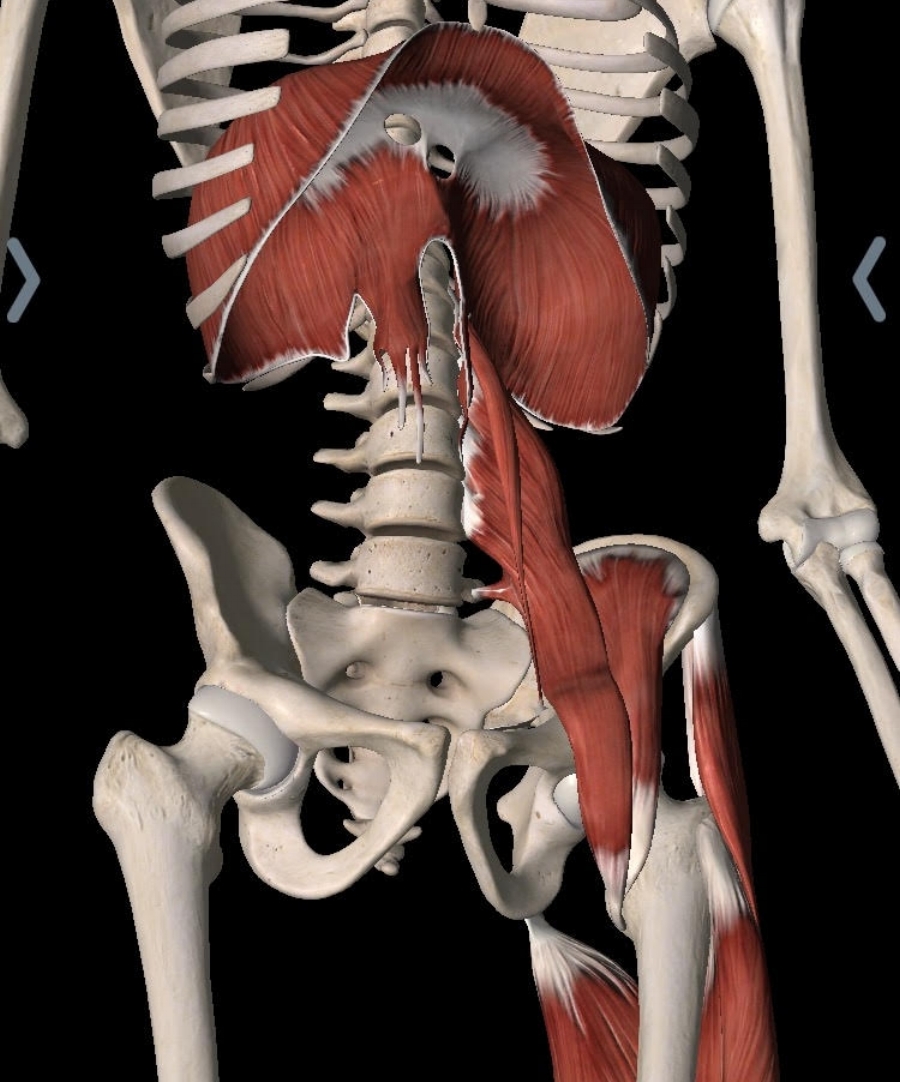
My first resistance towards PRI started here. I was concerned that if I had trouble accepting these foundational assumptions off the bat, would I be able to intellectually accept/apply other PRI interventions? Here's a picture of the "overactive" muscles of the LAIC:
From the "Essential Anatomy 5" app created by 3D4Medical. The different sizes of the left dome and right dome of the diaphragm and the slip of muscle which you see extending down the front of the spine are physiologic foundations on which many PRI principles are formed.
I can appreciate that there are natural visceral and musculoskeletal asymmetries between the right and the left side of the body, but to what degree can we assume these asymmetries are the cause for such specifically defined movement dysfunctions of several muscle groups across various joints of the body? Due to copyright issues, I won't be able to directly quote material from the course manual on this post, but there is frequent mention of how chronic muscle overuse, respiratory problems, limited airflow, weakness in specific parts of the abdominal wall, inflammation, scoliosis and fibromyalgia are all results of the LAIC pattern.
The Problems Continue
To me, the problem with tying anatomy too closely into pathology and dysfunction is that it's too rigid of a framework. Under PRI assumptions, a patient who presents with piriformis syndrome on the left side should be treated differently than someone who has it on the right side. Depending on the side, different muscles and different joints should be targeted for treatment due to different treatment goals. I'm not convinced that the treatment approach outlined by PRI can confidently make these assumptions for this diagnosis, which can present in a multitude of ways (peripheral neuropathy, referred by the lumbar spine, etc). Similar examples were outlined for "ilio-sacral strains" and hip bursitis.
A big part of Myokinematic Restoration treatment was being able to specifically target very specific structures, which also piqued my skepticism. It seems that a large part of PRI is being able to detect which muscles are activated and which muscles are inhibited to extremely acute detail.
Not just whether or not a gluteus maximus is firing, but whether the anterior fibers of the gluteus medius specifically are firing.
Whether or not internal abdominal obliques are engaged enough.
Whether or not the "left abdominal wall" is engaged.
To me the problem with this is very apparent and raised so many questions:
- How much visual acuity must one have in order to see this kind of specific EMG activity?
- How sensitive must someones tactile touch be in order to differentiate between the anterior fibers of a gluteus medius versus, say, the posterior fibers?
- What is the minimal effective dosage of EMG activity in a given muscle to produce the desired muscle contraction?
- To what degree must the discrepancies be between the transverse abdominis, internal/external abdominal obliques and rectus abdominis be before a core musculature contraction is considered "dysfunctional"?
- Is there a non-pathologic degree of muscular asymmetry that is allowed?
Focusing such a specific lens on morphology and kinematics might be effective in certain situations for neuromuscular re-education, but sometimes the goal should be just getting the desired task done under less specific parameters.
Some Positives
In general, I think the basic messages of PRI are sound ones. The human body is able to perform movements in somewhat predictable patterns. Sometimes these patterns can be more prevalent on one side than the other. We have a pretty good idea about the actions of muscles and what they do upon certain joints. Maybe by influencing our muscles through corrective exercises and/or through positioning, we can thereby change the way our bodies move through these aforementioned patterns. Based on the goal of the client/patient and the role of the PRI practitioner, whether he/she be a health care professional, personal trainer, strength & conditioning coach, we can encourage particular movement patterns while discouraging other ones. This is all well and good, and I like this about PRI--I mean, is this not the essence of physical therapy?
In my opinion some of the course's main strengths were the many exercises that placed patients in specific positions to encourage certain neuromuscular behaviors. I believe some of these can be very effective for correcting hip shifts during squats. However, I do think there needs to be more of a critical thinking process when it comes to evaluating an individual's movement and not automatically jumping to the conclusion that Muscles A, B and C are overactive, Muscles X, Y and Z are inhibited, and therefore this joint is externally rotated relative to that joint, and all this is because a small sliver of the distal attachment of the right sided diaphragm extends a bit further down on the spine than it does on the left.
What About Pain?
I'm not really sure how the role of pain treatment fits into all of this. In Zac Cupples' review of the same course (taught by a different instructor), he mentions that his instructor literally stated that "PRI does not treat pain." This was not mentioned in my course, despite spending a considerable amount of time treating various pathologies like piriformis syndrome, tibial stress fractures, pubalgia, etc. Rather than treating pain directly, the goal of PRI principles is to achieve a state of "neutrality", in which one can freely transition in between reciprocal patterns of motion without being compromised by faulty movement patterns.
This was also tricky for me to accept, as mitigating pain is a tremendous goal of almost all the patients that I see. Does someone being in pain make it such that I can't utilize PRI principles at all? Probably not, as I don't think PRI claims to be entirely comprehensive as far as treating pathology goes, nor do I think physical therapists treat their patients using only PRI methods. However, this does potentially complicate the clinical treatment approach of a health care practitioner whose patients are trying very much to get OUT of pain.
Final Thoughts
To use a popular metaphor, I definitely think certain PRI principles and interventions can be effective tools in the proverbial clinician tool-box. I just found it hard to reconcile certain foundational principles that in my eyes were reinventing the wheel and operating on a different treatment paradigm than most other philosophies I've encountered. If you're a physical therapist, chiro, or trainer and you disagree about PRI being as "unconventional" (whatever that means) as I've made it sound, that's fine too. There's going to be a lot of differences in thought depending on your educational background, values, professional scope of practice, business model, clients' goals and other treatment approaches that you subscribe to. However, there also needs to be some professional accountability with approaches like PRI that puts forth a lot of pathophysiologic assumptions for which I think many of my criticisms are valid or at least warrant more discussion.
As of now I don't plan on taking another PRI course, but being an open-minded clinician I'm willing to change my mind in light of emerging evidence or observing clinical outcomes that might convince me otherwise.